Lupine Publishers Group
Lupine Publishers
Menu
Research Article(ISSN: 2770-5447) 
Transverse Heart; A New Conversıon Predictor From offpump to on-Pump Surgery Volume 3 - Issue 4
Mehmet Ali Şahin, Mehmet Yokusoglu, Ertuğrul Özal and Erkan Kuralay*
- Alife Hospital Cardiac Surgery Department Ankara-Turkey
Received:May 3, 2021; Published: May 13, 2021
Corresponding author: Erkan Kuralay, Alife Hospital Cardiac Surgery Department Ankara-Turkey
DOI: 10.32474/ACR.2021.03.000168
Abstract
Introduction: Risk of conversion to on-pump surgery is one of the concerns about off-pump CABG surgery. Conversion to onpump surgery carries high morbidity and mortality risk. Our study aimed to investigate the relation between transverse heart and the risk of conversion to on-pump CABG .
Materials and Methods: Our study consisted of 3000 patients who underwent isolated off-pump CABG surgery between June 2010 and February 2020. All patients have at least one CABG in the Cx region. We have described vertical and transverse heart according to angle between the left anterior descending artery (LAD) and the left part of the sternal retractor.
Results: Our conversion rate was 7.1%. The average intensive care unit (ICU) stay was 1.17±0.10 days in successful off-pump surgery but 3.11±2.11 days in converted surgery (p=0.001).Average hospital stay was 4.35±1.44 days in off-pump surgery but 7.28±3.31 days (p=0.001) in converted surgery. Twenty-eight patients (1%) died in successful off-pump surgery, but 12 patients (5.6%) died in off-to-on converted surgery(p=0.001).Multivariate analysis has shown that ejection fraction less than 30% (LVEF<30%), cardiomegaly, congestive heart failure (CHF), and transverse heart as a predictor of conversion.
Conclusion: Conversion to off-to-on surgery still has contraversial results. Analysis of predictors preoperative and inspection of heart just before coronary anastomosis should be carefully done. The transverse heart was the statistically significant off-to-on conversion predictor of our study.
Keywords: Off-Pump Surgery; Vertical Heart; Transverse Heart
Introduction
It has been shown that unfavorable outcomes may be seen during conversions from off to on-pump CABG in a few clinical[1,2] and retrospective[3–10] studies. Adverse outcomes including increased early [1–4], [6–14] and late [2,3,8,10] mortality and myocardial infarction risk [4,14,15], stroke [3,6,7,16], need intraaortic balloon pump [13,14,16], longer ICU [13,14,16], and hospital stay [3,14-16], more red blood cell transfusion requirement [1,8,14,16], increased reoperation risk due to bleeding [6,7,13], respiratory failure [6,7,13], increased dialysis requirement due to renal failure [6,15], increased ventilation support requirement [3,15,16], increased inotropic agent use [1,14], and more hospital readmissions [17].The overall conversion rate was found as 4.9% [18,19] in meta-analyses and ranged from 0-19.4% in published series whereas this rate was found as lower as 2.2% in the Society of Thoracic Surgeons national database reports [20]. However, it remains unclear which risk factors are associated with the conversion and whether these conversions are potentially preventable, since most studies have failed to evaluate these predictors. A variety of risk factors including poor coronary targets [21-23], lower left ventricular ejection fraction [16,24], congestive cardiac failure [4,24], surgeon’s experience [2,4,5,16] non-use of a positioning device [7,13], prior CABG [4,6], prior myocardial infarction [6,21], diabetes [6,22] chronic obstructive pulmonary disease [13,15], preoperative atrial fibrillation [10], urgent surgery [6], mitral regurgitation (MR)[13], left ventricular hypertrophy [6], higher Newyork Heart Association(NYHA) angina class [6], LMCA stenosis [16], smaller [6] or larger [1] body surface area have been identified in the literature [21].We prospectively compare the adverse effects of transverse and vertical heart anatomy on outcomes associated with conversion from off to on-pump CABG. We think that transverse heart anatomy may be one of the factors likely to be responsible for adverse outcomes related to conversions from off to on-pump CABG.
Materials and Methods
Definition of Terms
ELECTIVE OPERATION is a procedure performed for a hemodynamically stable patient when brought to the operating room, regardless of angına class or admission status.
EMERGENCY OPERATION is a procedure performed for an acutely ischemic or hemodynamically unstable patient requiring an immediate operation.
HEMODYNAMIC COLLAPSE is a condition characterized by severe and sustained derangements in patient’s vital signs, refractory to pharmacological therapy, and likely to result in death without the institution of CPB; excludes transient hemodynamic derangements.
ISCHEMIC COLLAPSE is defined as the primary or inciting cause of the hemodynamic collapse is myocardial ischemia.
MECHANICAL COLLAPSE is a condition due to the primary or inciting cause of the hemodynamic collapse is the alteration of the normal geometry or architecture of the heart from mechanical manipulation (compression, retraction, elevation).
EARLY CONVERSION is defined as conversion before coronary arteriotomy (intramyocardial or small coronary arteries) LATE CONVERSION is defined as the conversion occur during or just after coronary arteriotomy or during performing coronary anastomosis
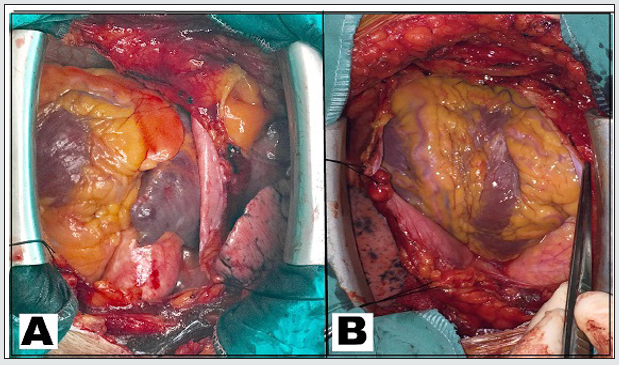
CARDIOMEGALY is that cardiac diameter to thoracic cavity diameter ratio on posteroanterior chest x-ray greater than 0.5(14) TRANSVERSE HEART is that angle of LAD artery direction to the left arm of the sternal retractor is more than 45 degree in neutral heart position (Figure-1A)
VERTICAL HEART is that angle of LAD artery direction to the left arm of the sternal retractor is between 0-45 degree in neutral heart position (FIGURE-1B)
RIGHT HEMITHORAX ADHESION is that dense adhesion of lung to the right chest wall
Figure 1: A)Transverse Heart is that angle of LAD artery direction to the left arm of the sternal retractor is more than 45 degree in neutral heart position. B)Vertical Heart is that angle of LAD artery direction to the left arm of the sternal retractor is between 0-45 degree in neutral heart position..
Exclusion Criterias
Isolated coronary bypass surgery was performed in all patients. Additional cardiac surgery requirements were evaluated as exclusion criteria. Patients suffering from moderate degree MR were also excluded from the study because of even mild degree MR would cause serious complication during left side coronary surgery [13].Redo coronary surgery were also excluded due to excessive dissection requirement before coronary anastomosis [4- 6].The early conversion was accepted as exclusion criteria due to surgery is done in the on-pump. All patients were classified as late conversion group patients. Patients characteristics were detailed in Table-1.
Patients
We have been performing off-pump CABG since 2010.Currently our routine preference for coronary artery bypass surgery is offpump technique. We have carried out 3000 isolated CABG surgery, between 2010-2020.There was at least one coronary artery anastomosis requirement at the Cx region in our patients. Patients with isolated LAD and right coronary artery (RCA) disease were not included in the study due to the relatively low conversion rate.
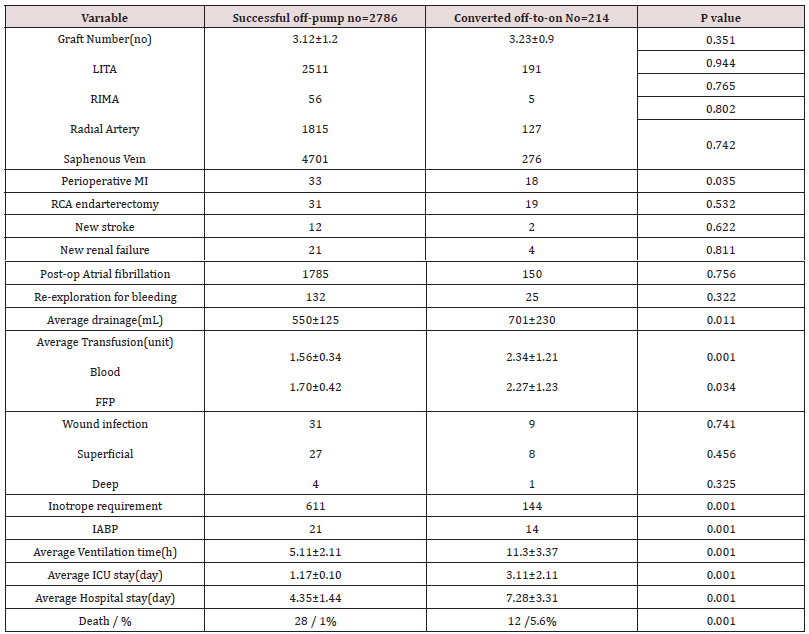
Table 1: Patient Characteristics.
LVEF=left ventricular ejection fraction;MI=myocardial infarction;NYHA=New York Heart Association; PVD=peripheral vascular disease,CRF=chronic renal failure,COPD=chronic obstructive pulmonary disease, LMCA=left main coronary artery,CHF=congestive heart failure
Surgical Technique
All surgical procedures were performed by two surgeons(EK and EO). Patients were routinely kept normothermic and in the supine position. Pump was ready but kept it dry. Central venous catheter was commonly inserted into the jugular vein. Median sternotomy was performed to harvest the LITA/RITA grafts. Both Radial artery (RA) and saphenous vein (SV) grafts were used. Heparin (2mg/kg) was administered before ligation of the distal part of the LITA and the ACT was maintained between 200-300 seconds during the operation. Right pleurotomy and a deep vertical pericardiotomy were performed to create space for entering of the heart into the right thoracic cavity. Operating table was positioned at Trendelenburg position to increase the inflow of the heart. Epicardial-stabilizations were routinely used for all anastomosis. The suction paddles are placed close to and parallel to the coronary artery to obtain maximum immobilization and minimum compromise of muscle function. Suction is activated in each paddle separately and fixed at the target site once suction is –400 mmHg. Several commercially available vacuum stabilization devices(mostly Octopus) were used. Commercially available all apical vacuum devices(mostly Starfish) were routinely used for posterolateral and posterior descending coronary arteries. Coronary arteries were taped proximally and distally by silastic sutures. Coronary shunts were not routinely used. Additional intravenous heparin was administered (with an ACT>480 seconds), and procedure was converted to on-pump, when hemodynamic instability developed. We routinely used LITA grafts for LAD, but LITA was anastomosed to the first diagonal artery in 23 patients. LITA anastomosis was firstly performed between 2010-2013 after then Cx-region anastomoses were firstly done to avoid streching of the LITA graft when deviating the heart to the right thoracic cavity. Apical vacuum devices were routinely used for circumflex posterolateral branches. After performing circumflex anastomosis, LITA anastomosed to LAD, and diagonal artery anastomoses were completed. RCA and its branches revascularization were done lastly. SV was routinely preferred in emergency conditions and proximal anastomosis was done to ascending aorta with 6/0 polypropylene just after distal anastomosis, to avoid severe ischemic complications. Innominate artery (IA) was used for proximal anastomosis in 43 patients. Graft blood flow rates(mL/min) were measured by using Doppler ultrasound after all anastomosis was completed, and protamine administrated. When ischemic collapse developed during distal anastomosis procedure we placed intracoronary shunt and kept the heart neutral position and waited until maintaining hemodynamic stability. We routinely waited for at least five minutes until the signs of ECG recovered before a second intervention. Hemodynamic collapse was also a serious problem. We wait until hemodynamic parameters return to normal. If both ischemic and hemodynamic collapse persists, then we prefer converting to on-pump surgery. In the presence of serious hemodynamic collapse during the waiting period, we performed a hand massage to the heart and placed a purse-string while the pump lines were prepared. We performed RCA closed endarterectomy through limited arteriotomy in fifty patients in the beginning period of our experience. We also preferred revascularization of the right ventricle branch of the right coronary artery since June 2015. Porcelene aorta was found in 43 patients. We routinely prepared and taped the IA before making coronary anastomosis. The IA was extensively mobilized to supply a place both arterial return in case of conversion and proximal anastomosis of grafts. SV graft was anastomosed to the IA. Proximal anastomosis of other grafts were done on the the main SV.
Statistical Analysis
Data were expressed as mean±standard deviation. Statistical analysis was performed using IBM SPSS ver. 20.0 (IBM Corp., Armonk, NY, USA). Clinical data were expressed as mean values standard deviation. Differences were analyzed by using Fisher’s exact test, x2-test, unpaired Student’s t-test and Mann–Whitney test. We examined the effects of the variables on Off-to-On conversion by calculating odds ratios (OR) in univariate analyses for all CABG patients. Variables for which the unadjusted p-value in logistic regression analysis were identified as potential risk markers and included in the full model. We conducted stepwise multivariate analyses by using logistic regression.
Results
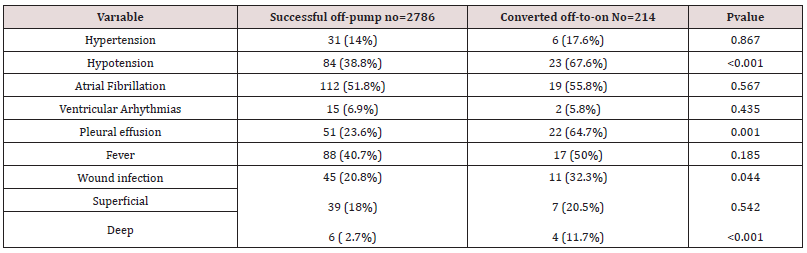
There was no significant difference between the two groups in terms of the average graft number. Average graft number was 3.12±1.2 on successful off-pump surgery whereas was 3.23±0.9 on converted on-pump surgery patients. Perioperative MI was found significantly (p=0.035) higher in off pump group patients compare to converted group patients (33 and 18 respectively). New strokes were observed in 12 of the successful off-pump group patients whereas only two of the converted group patients had new strokes(p=0.322). New renal failure development was recorded in 12 (four of them required hemodialysis) of the successful off-pump group patients. New renal failure was developed in four (two of them required hemodialysis) of the converted group patients. Rvision due to bleeding was performed in 132 of the successful off-pump group patients whereas only 25 of the converted group patients underwent re-operation due to bleeding. The average drainage amount was noted as 550±125 ml in off-pump surgery group patients, whereas this amount was noted as 701±230 ml in converted surgery group patients. There was a significant(p=0.011) difference between the groups in terms of drainage volume. The average packed blood (PBC) transfusion was reported as 1.56±0.34 units in off-pump group patients and 2.34±1.21 units on converted group patients (p=0.001). There was a significant( p=0.034) difference between two groups in terms of average Fresh Frozen Plasma (FFP) transfusion requirement (1.70±0.42 and 2.27±1.23 respectively). Inotropic agent supplement was required in 21%(611) of the successful off-pump group patients, but 67%(144) of the converted group patients were given an inotropic agent supplement(p=0.001). Intra-Aortic Balloon Pulsation was placed in 21 of the off-pump group patients and in 14 of the converted group patients (p=0.001). Transient postoperative atrial fibrillation was developed in 1785 of the off-pump group patients and in 150 of the converted group patients (p=0.756).The average ventilation duration was 5.11±2.11 hours in off-pump group patients, and 11.3±3.37 hours in converted group patients (p=0.001). The average length of ICU stay was 1.17±0.10 days in successful off-pump group patents, and 4.35±1.44 days in the converted group patients. Mortality rate was 1%(28) in successful off-pump group patients and 5.6%(12) in the converted group patients. The hospital readmission rates within 30 days after surgery were 7.7% in successful off-pump group patients and 15.7% in the converted group patients(p<0.001). The most common cause of hospital-readmission was hypotension (p<0.001) and wound infection (<0.001). The causes of hospital-readmission were detailed in Table-2, 3.
ICU=intensive care unit;LITA= left internal thoracic artery;RITA= right internal thoracic artery,FFP=fresh frozen plasma,IABP=intra- aortic balloon pump.
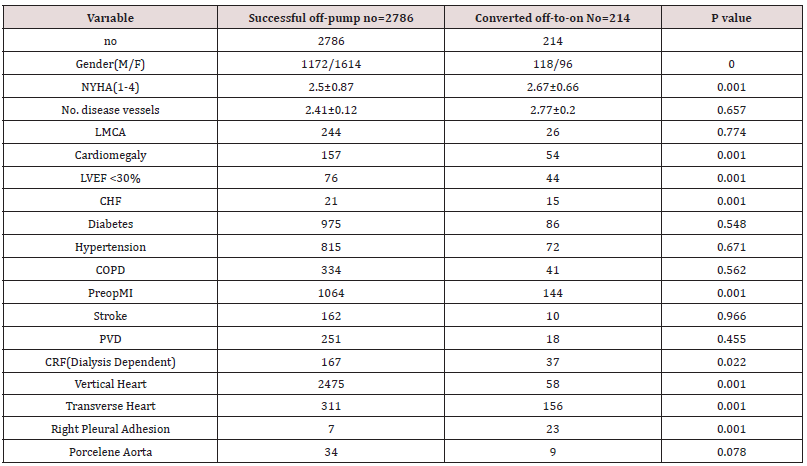
Predictors of off-to-on conversion
We statistically analyzed 15 variables which likely to be a predictor of off-to-on conversion during the CABG procedure. According to univariate analysis of the parameters factors including age (p=0.211;OR=0.74), NYHA (p<0.001;OR=3.32), LVEF<0.30 (p=0.003;OR=0.95), preoperative MI (p=0.795;OR=0.99), diabetes (p=0.895;OR=1.41), LMCA (p=0.310;OR=0.82), LITA (p=0.154;OR=0.46), hypertension (p=0.872;OR=1.06), renal failure (p=0.010,OR=3.15), cardiomegaly (p=0.005;OR=2.12), average graft number (p=0.670;OR=0.73), vertical heart (p=0.985;OR=1.06), transverse heart (p<0.001;OR=4.75), right pleural adhesion (p=0.011;OR=3.54), CHF (p=0.001,OR=1.13) were found as a predictor of off-to-on conversion and shown in Table-2. The stepwise multivariate analysis of these parameters showed that variables such as LVEF<30 (p=0.002,OR=0.93), CHF (p=0.005:OR=1.05), cardiomegaly (p=0:005;OR=3.15), transverse heart (p<0.001;OR=4.11) were independent risk factors for off-toon conversion. The univariate and multivariate analysis of patient and surgery dependent variables likely to be the effect on off-to-on conversion during CABG were detailed in Table-4.
Table 4: Variables Effects on The Off-To-On Conversion Based On Univariate And Multivariate Logistic Regression Analyses.
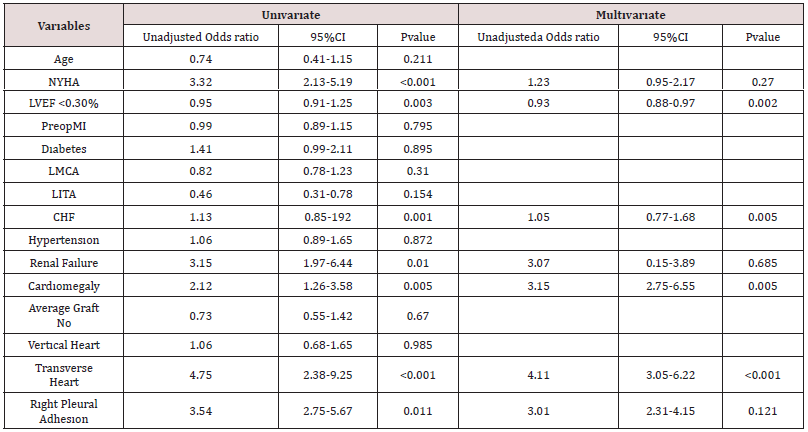
NYHA=Newyork heart Association, LVEF<30%=left ventricle ejection fraction less than 30%,LMCA=left main coronary artery, MI=myocardial infarction, LITA: left internal thoracic artery, CHF=congestive heart failure.
Comments
We know that mortality related to coronary surgery mostly results from organ deficiency except for heart failure. Myocardial failure as a cause of mortality was seen in less than 50% of our patients. The other early deaths were mostly due to additional organ failures. Our patients’ profiles have considerably changed in recent decades of CABG surgery. More advanced age and co-existence of organ failure are common characteristics of our patients in recent years. Nowadays, percutaneous coronary interventions (PCI) is more commonly preferred in coronary patients worldwide. Thus more complicated cases in terms of limited runoff coronary vessels are more frequently encountered. Classical on-pump cardiac surgery has some deleterious effects due to extracorporeal perfusion and inadequate myocardial preservation and may lead to complications such as myocardial and brain ischemic injury, renal failure, and other organ deficiencies. Surgeons mostly prefer offpump CABG surgery to avoid these complication risks and mortality. However, off-pump surgery has its own difficulties. Myocardial ischemia and hemodynamic disturbance or both may cause serious complications during off-pump surgery. Especially the Cx region of coronary vessel surgery becomes much more difficult in selected patients [2-17]. Skilled surgeons and their teams have developed several technical tip and tricks to avoid hypotension and prolonged ischemia during off-pump CABG. Despite all technical innovations, conversion from off-pump to on-pump may need to perform complete myocardial revascularization.
We think the “critical topic” is complete revascularization. Many surgeons prefer incomplete myocardial revascularization to avoid complication during off-pump surgery. It’s well known that incomplete myocardial revascularization may cause ischemic complications after surgery and patients need additional PCI interventions [25]. The overall conversion rate was reported ranging from 0% to 19.4% [18-20]. Edgerton JR. [4] reported that surgical experience was the most important factor of off-pump surgery.Our CABG procedures were performed by two senior surgeons. Each of these surgeons has performed >500 coronary surgeries per-year. Despite our considerable experience, the conversion rate is about 7% in surgical procedures on three coronary vessels. This rate was noted as 1.12% for procedures including two-vessel (both LAD and RCA), and 0,5% for the a single artery(LAD) in our series. We have routinely explored all coronary vessels after pericardioyomy and prefer conversion to on-pump surgery in the presence of conditions such as intra-myocardial LAD, severely calcified coronary vessels, and small vessels in the first exploration. Conversion from off-toon surgery has some disadvantages except for early conversion conditions. Particularly, conversion in emergency conditions has multiple deleterious effects and carries high morbidity and mortality risk. Multiorgan failure due to persistent ischemia and prolonged hypertension, increasing transfusion requirements, and increased vulnerability to infection seems to be related to increased morbidity and mortality risk. The development of perioperative MI was also found higher in these group patients. It is well known that blood flow rate measurement in grafts is extremely helpful to reduce the technical mistakes. We have perform re-anastomosis in 95 patients due to a low blood flow rate in the graft. Tabata M.[13] has reported a 14.3% operative mortality rate in patients undergoing emergency conversion whereas 1.2% mortality rate in off-pump surgery group patients. Similar mortality rates were also reported in several studies [7-21]. Hospital re-admissions within 30-days after surgery were significantly more common in our conversion patients. The presence of porcelene aorta is known as an absolute indication of off-pump surgery.
Many surgeons prefer performing incomplete coronary revascularization procedures to avoid complication risks whereas experienced surgeons may also use LITA artery for proximal anastomosis. We always respect the divine configuration of LITALAD. We routinely prefer to use IA for proximal anastomosis in patients with multi-vessel disease requiring more than two proximal anastomosis on LITA. We placed proximal anastomosis of one of the left side SV graft to innominate artery then proximal anastomosis other grafts were placed the saphenous located on IA. Rightward disposition of heart may cause a different degree of MR. Severe MR due to cardiac displacement may cause acute pulmonary edema [13]. Acute pulmonary edema occurs in the presence of prolonged cardiac displacement associated with MR lead to congestion in the left ventricle consequently causes severe hemodynamic instability. Tabata M.[13] has shown that severe MR may develop even in the presence of a completely competent mitral valve preoperatively. The presence of the dense adhesions in the right pleural cavity is one of the most important unfavorable variables during off-pump surgery. Dense adhesions in the right hemithorax may compress the right atrium and ventricle particularly in the deviation of heart toward to right side during the off-pump surgery. Compression of right atrium and ventricle may cause serious hypotension despite reverse Trendelenburg position. Dense adhesions in right hemithorax could not be dissected in our 30 patients. Conversion to on-pump surgery was required in 23 of these patients.
There was no statistical significance of the presence of the dense adhesion in the right hemithorax according to the results of multivariate analysis. The most comprehensive analysis of conversion mortality was reported by Edgerton JR.[4] Their subgroup analyses showed that a fivefold increase in mortality rate depending on whether the conversion was elective(6.1%) or emergency(32.1%), and almost 12-fold higher mortality depending on whether it was early(3.1%) or late (34.5%) respectively. Among emergency conversions alone, the mortality rate increased from 0% to 45%, depending on whether they occurred early or late. Namely outcomes of conversion to on-pump surgery in emergency conditions considerably change depending on whether this occurs before or after the commencement of anastomosis. Early conversion technique was preferred in the conditions such as an uncontrollable severe hemodynamic disturbance during the disposition of the heart, small coronary arteries, diffuse atherosclerotic vessels, and intramyocardial coronary vessels.
As mentioned above the myocardial injury and heart disposition are two principal causes of conversion to on-pump surgery. Myocardial ischemia was mainly dependent on the anastomosis site on the coronary artery and degree of the coronary stenosis. Myocardial ischemia commonly occurred in proximal part of coronary artery occlusion by silastic tapes. More proximal part preference meant more ischemia risk. Intracoronary shunt were frequently required in surgical procedures containing the body part of the RCA. Myocardial ischemia during silastic occlusion is much more common in patients with a relatively low degree coronary stenosis. Predictors related to unfavorable outcomes of conversion to on-pump surgery are extremely important in terms of high morbidity and mortality risk of conversion. We found that transverse heart was relatively new predictor. Off-pump surgery is relatively easy surgical procedure with a low conversion rate in the vertical heart. Disposition of heart is mostly known as a mechanical hemodynamic deterioration factor in transverse heart. Rightward disposition of heart may cause right ventricle outflow tract and pulmonary artery kinking in transverse heart anatomy [26]. Distortion of the heart may cause severe MR which results in the development of acute pulmonary [13]. Our results showed that the presence of the transverse heart is one of the significant predictors of conversion to the on-pump procedure. Currently, we do not prefer off-pump surgery in the presence of the transverse heart.
Conclusion
Conversion to on-pump surgery is a challenging problem due to unfavorable outcomes. Thus predictors likely to be responsible for conversion should be considered before decision making for CABG surgery. Transverse heart is a reasonable predictor of conversion and should be considered as early conversion marker.
References
- Legare JF, Buth KJ, Hirsch GM (2005) Conversion to on pump from OPCAB is associated with increased mortality: results from a randomized con- trolled trial. Eur J Cardio-Thoracic Surg 27(2): 296-301.
- Novitzky D, Baltz JH, Hattler B, Collins JF, Kozora E, et al. (2011) Outcomes after conversion in the Veterans Affairs randomized on versus off bypass trial. Ann Thorac Surg 92: 2147-2154.
- Chowdhury R, White D, Kilgo P, Puskas JD, Thourani VH, et al. (2012) Risk factors for conversion to cardiopulmonary bypass during off-pump coronary artery bypass surgery. Ann Thorac Surg 93(6): 1936–1941.
- Edgerton JR, Dewey TM, Magee MJ, Herbert MA, Prince SL, et al. (2003) Conversion in off-pump coronary artery bypass grafting: an analysis of predictors and out comes. Ann Thorac Surg 76(4): 1138-1142.
- Hemli JM, Patel NC, Subramanian VA (2012) Increasing surgical experience with off-pump coronary surgery does not mitigate the morbidity of emergency conversion to cardiopulmonary bypass. Innovations 7(4): 259-265.
- Jin R, Hiratzka LF, Grunkemeier GL, Krause A (2005) Aborted off- pump coronary artery bypass patients have much worse outcomes than on-pump or successful off-pump patients. Circulation 112 (9 Suppl): I332–1337.
- Patel NC, Patel NU, Loulmet DF, McCabe JC, Subramanian VA (2004) Emergency conversion to cardiopulmonary bypass during attempted off- pump revascularization results in increased morbidity and mortality. J Thorac Cardiovasc Surg 128(5): 655-661.
- Reeves BC, Ascione R, Caputo M, Angelini GD (2006) Morbidity and mortality following acute conversion from off-pump to on-pump coronary surgery. Eur J Cardiothorac Surg 29(6): 941–947.
- Soltoski P, Salerno T, Levinsky L, Schmid S, Hasnain S, et al. (1998) Conversion to cardiopulmonary bypass in off-pump coronary artery by- pass grafting: its effect on outcome. J Card Surg 13(5): 328-334.
- Maroto CLC, Carnero M, Cobiella FJ, Alswies A, Ayaon A, et al. (2015) Off-pump to On-pump emergency conversion: incidence, risk factors, and impact on short and long-term results. J Card Surg 30: 735-745.
- Carrier M, Perrault LP, Jeanmart H, Martineau R, Cartier R, et al. (2003) Randomized trial comparing off-pump to on-pump coronary artery by- pass grafting in high-risk patients. Heart Surg Forum 6(6): E89–E92.
- Mathur AN, Pather R, Widjanarko J, Carrier RC, Garg R (2003) Off-pump coronary artery bypass: Sudbury experience. Can J Cardiol 19: 1261-1269.
- Tabata M, Takanashi S, Horai T, Fukui T, Hosoda Y (2006) Emergency conversion in off-pump coronary artery bypass grafting. Interact Cardiovascular Thorac Surg 5(5): 555-559.
- Vassiliades TA, Nielsen JL, Lonquist JL (2002) Hemodynamic collapse during off-pump coronary artery bypass grafting.Ann Thorac Surg 73(6): 1874-1879.
- Landoni G, Pappalardo F, Crescenzi G, Aletti G, Marchetti C, et al. (2007) The outcome of patients requiring emergency conversion from off-pump to on-pump coronary artery bypass grafting. Eur J Anaesthesiol 24(4): 317-322.
- Hovakimyan A, Manukyan V, Ghazaryan S, Saghateyan M, Abrahamyan L, et al. (2008) Predictors of emergency conversion to on-pump during off-pump coronary surgery. Asian Cardiovas Thorac Ann 16: 226-230.
- Li Z, Amsterdam EA, Danielsen B, Hoegh H, Young JN, et al. (2014) Intraoperative conversion from off-pump to on-pump CABG is associated with increased 30-days hospital readmission. Ann Thorac Surg 98(1): 16-22.
- Mukherjee D, Ashrafian H, Kourliouros A, Ahmed K, Darzi A, et al. (2012) Intra-operative conversion is a cause of masked mortality in off-pump coronary artery bypass: A meta-analysis. Eur J Cardiothorac Surg 41: 291-299.
- Urso S, Sadaba JR, Pettinari M (2012) Impact of off-pump to on-pump conversion rate on post-operative results in patients undergoing off-pump coronary artery bypass. Interact Cardio Vasc Thorac Surg 14(2): 188-193.
- Puskas JD, Edwards FH, Pappas PA, O’brien S, Peterson ED, et al. (2007) P. Off-pump techniques benefit men and women and narrow the disparity in mortality after coronary bypass grafting. Ann Thorac Surg 84(5): 1447-1454.
- Mukherjee D, Ahmed K, Baig K, Patel VM, Darzi A, et al. (2011) Conversion and safety in off-pump coronary artery bypass: a system failure that needs re-emphasis. Ann Thorac Surg 91(2): 630-639.
- Pullan M, Oo A, Poullis M (2015) Off-pump conversion: in-hospital mortality and long-term survival. Thorac Cardiovasc Surg 5: 151-159.
- Lund O, Christensen J, Holme S, Fruergaard K, Olesen A, et al. (2001) On-pump versus off-pump coronary artery bypass: independent risk factors and off-pump graft patency. Eur J Cardiothorac Surg 20(5): 901–907.
- Mishra M, Shrivastava S, Dhar A, Bapna R, Mishra A, et al. (2003) A prospective evaluation of hemodynamic instability during off-pump coronary artery bypass surgery. J Cardiothorac Vasc Anesth 17:452-458.
- Jones EL, Craver JM, Guyton RA, Bone DK, Hatcher CR, et al. (1983) Importance of complete revascularization in performance of the coronary bypass operation. Am J Cardiol 51(1): 7-12.
- Puskas JD, Williams WH, Duke PG, J R Staples, K E Glas, et al. (2003) Off-pump coronary artery bypass grafting provides complete revascularization with reduced myocardial injury, transfusion requirements, and length of stay: A prospective randomized comparison of 200 unselected patients undergoing off-pump versus conventional coronary artery bypass grafting. J Thorac Cardiovasc Surg 125(4): 797-808.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...